Abstract
The musculature of the face is innervated by cranial nerves, each with a motor, sensory and/or both function. The Facial nerve (FN) is responsible for the motor innervation of the muscles of the face. Some branches of the trigeminal nerve are responsible for the sensory part of the facial muscles and other branches act on the motor part of the chewing muscles. Traumatic Facial Paralysis (TFP) is the one where there was section or traction or compression or ischemia of the FN, in surgery for tumor resection or trauma in general. In this case occurs the nerve’s section in one surgery. Facial Paralysis (FP) can be evaluated subjectively through the House and Brackmann classification scale (HB) [1]. It is considered a chronic FP when it persists for a period longer than 6 months and leaves sequelae, such as synkinesis, contractures and lack of complete innervation of some nerve branches. Some patients who evolve with chronic FP may also evolve with alteration of the occlusal plane. The occlusal plane is the meeting point between the antagonist teeth, plane that is in the final stop of the masticatory cycle. The rehabilitation of this plan is performed according to the needs of each patient, in this case was made through implant prostheses.
1. Introduction
Paralysis is the loss of movement in some territory of the body, Facial Paralysis is the loss of movement in some territory of the face. Facial paralysis can be of central or peripheral origin, depending on the location of the nerve.
Central Facial Paralysis is a medical emergency because it can result from a stroke. It involves the lower third of the face and can lead to loss of strength of the arms and legs on the opposite side, the injury occurred above the core of the facial nerve.
The facial nerve (FN) is responsible for facial mimic. Peripheral facial paralysis is when the affected part of the nerve is below the facial nucleus or within the temporal bone canal, in the most peripheral part of the nerve. All face muscles are innervated by the seventh cranial nerve, the FN [2].
The causes of Peripheral Facial Paralysis are several. Pregnancy, puerperium, hypertension, viral, bacterial and traumatic diseases, neoplastic and congenital. The most common traumatic causes of facial paralysis are tumor resections [3], as in the case that follows and may also result from temporal bone fractures (falls) or penetrating trauma, including iatrogenic injury. When FN occurs, it cannot perform its functions of traction of the muscles of the face.
In the human body, FN is one of those that suffer most from paralysis, due to the extensive bone canal through which it passes within the temporal bone. If for some reason inflammation occurs, the sheaths involved in conducting the nerve stimulus become insensitive and the terminals that should exercise muscle stimulation, cannot perform [4]. The individual appearance and facial expression of each person is based on the musculoskeletal system of the face [2]. This system is composed of the bones in the anterior portion of the skull, known as the viscerocranium, and the muscles, which include those of the facial muscles, innervated by the seventh cranial nerve FN and two masticatory muscles (masseter and temporal) that are innervated by the V3 branch of the trigeminal nerve.
Some muscles of the face are inserted into bones and others into the muscles or tendons themselves. This complex musculature contributes to the functioning of the organs of the orofacial senses and in the mediation of emotional and affective states (face and expression). Other components of soft tissues also act, such as fascias and fat [2]. When peripheral Facial Paralysis occurs, this complex structure suffers effects beyond the hypotonia of the muscles of the affected side and the chewing muscles are not hit.
The dental surgeon works in the occlusal plane. Occlusal plane, by definition, is the meeting point of the antagonist teeth, the plane where it is located at the final stop of the chewing cycle. According to some findings, the stability of the occlusal platform can cause the healthy side to exert less action on the paralyzed side, reducing sequelae [5]. Effective dental contact during swallowing and chewing in these patients is important to avoid exacerbated traction on the healthy side and worsening the degree of paralysis.
Good oral health should include absence of facial pain, ability to ingest, chew and swallow food. This should also contribute to communication, especially when talking and smiling, which have the potential to increase people’s self-esteem [6]. Tooth loss can be considered as a way out of the failure of a conservative treatment previously performed and can constitute an event of strong impact, which, in addition to causing functional damage, is able to unbalance the psychic and social organization of people [7]. In this context, oral rehabilitation, by means of prosthesis, can have a positive effect on the behavior of these patients, since it restores properly the masticatory function as well as the aesthetic, contributing to an improvement in the social interaction of these individuals and in their quality of life.
Facial Paralysis is graded by the HB scale and varies from I to VI, according to the degree of function. The face muscle does not perform function due to lack of nerve conduction. Chronic paralysis is that one which after 6 months, does not improve [8].
In the case that will be presented, the paralysis has traumatic cause, resulting from a resection of the FN after surgery of a Glomus tumor, tympanic jugulum and there was loss of the movements of the right side of the face, with degree V HB and presented unilateral anacusia, confirmed by audiometry performed in the outpatient service.
The patient already had tooth loss, but over time it worsened and suffered dental fractures. When the rehabilitation, which took place 10 years after the surgery she presented edentulous. Unilateral facial paralysis leads to difficulties in chewing and the lack of final stop of the masticatory cycle, when the teeth are absent, causes effective changes both in the face muscles and changes in chewing in adults [9].
Surface electromyography examination captures the electrical activity of the facial muscles at rest and in muscle contraction. Surface Electromyography in TFP proved to be an objective method, in which it is possible to analyze the action potential of muscle fibers and quantify their recovery [10]. It is performed with individuals sitting in a chair with a vertical backrest and with their feet supported on a rubber mat. The skin must be cleaned with 70 % alcohol to obtain better attachment of the electrodes [11].
The surface electrodes should be adhered to the region of the frontal muscle, orbicular of the eye (eyelid portion), orbicular of the mouth and elevators of the upper/ zygomatic lip. The equipment used was the NewMIOTOOL face – eight channels (Miotecₒ) integrated into the Miograph 2.0 software, with two surface electrodes in each region. The tests for recording surface electromyographic activity involve the movements of all segments of the face, focusing mainly on: forehead elevation, closing of the eyes, lip protrusion (beak) and lip retraction (smile).
2. Case report
A 35-year-old female patient, with no clinical history of chemical dependency or psychosocial history, presented to the UNIFESP Facial Nerve Outpatient Clinic (*) with facial paralysis of traumatic origin, due to resection of the glomus jugulo tympanicus. She had a removable prosthesis and several missing teeth, with grade V facial paralysis on the right and anacusis on the same side. An attempt was made to anastomose the hypoglossus with the facial nerve, but the nerve stump was not found and the objective of the surgery was not achieved. (*) UNIFESP Universidade Federal de São Paulo.
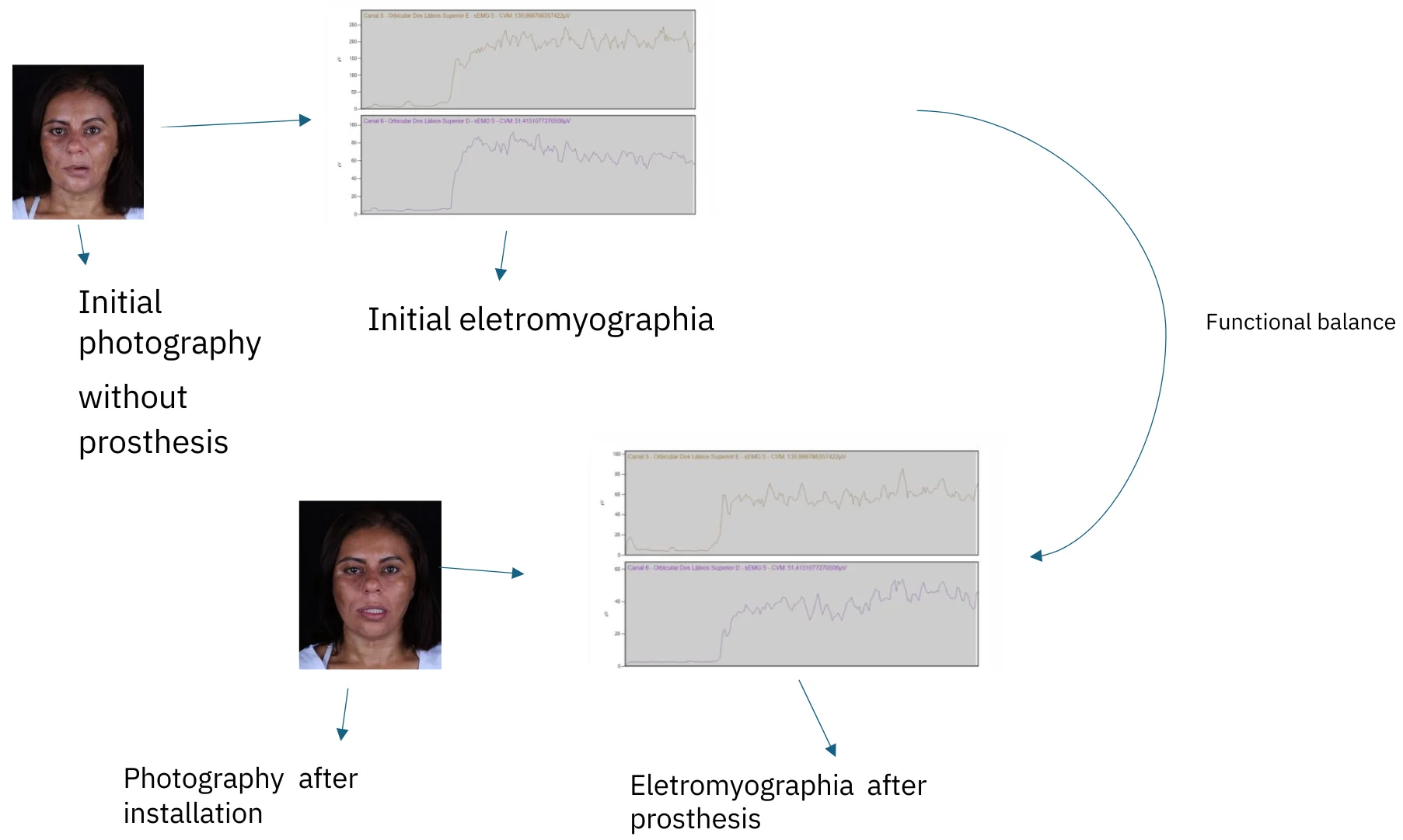
After 10 years, that is, at the age of 45, she sought the service again, completely edentulous and apparently more disfigured. In an attempt to restore quality of life and chewing, the installation of prostheses on implants was planned. Before installing the prosthesis, surface electromyography was requested to assess the state of the muscles innervated by the facial nerve and classification according to HB. Extraoral photographs were also taken. After installing the prosthesis implants, new photographs and a new electromyography were taken.
3. Results
Electromyograph channels were placed on the right and left side of the ocular segment, zygomatic segment, forehead segment and orbicular segment. They were measured, comparing the right and left sides and an average was found.
Surface electromyography: the forehead segment presented index IEMG 0.17, that is, below normal pre and post dental implant.
For the eye segment, as well as for the zygomatic muscles segment, the indexes were below the normal, pre-dental implant and did not change after dental implantation.
We will only present the orbicular graph, which has shown to be altered.
Segment labial before implant prothesis is shown in Fig. 1. The labial segment, the normality interval is 0.79-1.28. Pre dental implant the patient presented IEMG of 0.35. Channel 5 Upper lip orbicularis – E – sEMG S – CVM 135966766357422 uV (normal side). Channel 6 Upper lip orbicularis – D – sEMG S – CVM 514151077270508 uV (paralysis side).
Fig. 1Segment labial before implant prothesis
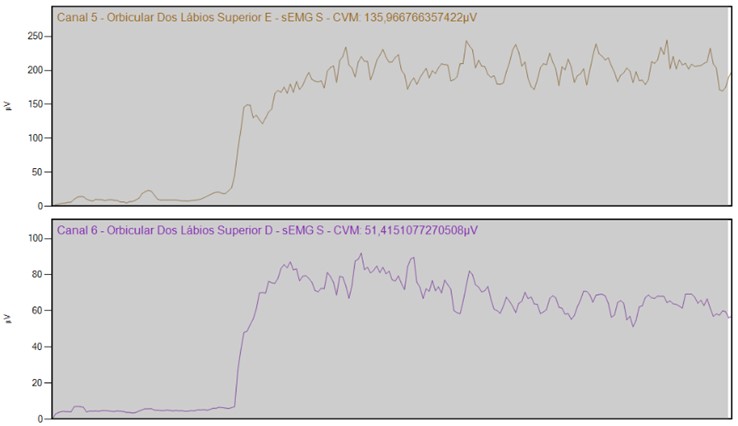
a)
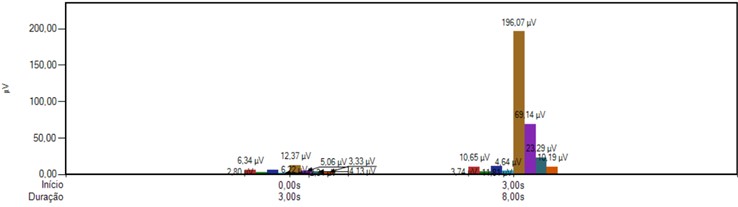
b) EMG average per contraction
Fig. 1 shows that in the labial segment, the normality interval is 0.79-1.28. Pre implant prosthesis the patient presented IEMG of 0.35.
Segment labial before implant prothesis is shown in Fig. 2. Evaluation of the Orbicular muscles of the Lips’ surface (bilateral) in maximum contraction. IEMG of normality 0.79 to 1.28 (10). Current IEMG: 0,35. The value is below normal. Channel 5 Upper lip orbicularis – E – sEMG S – CVM 135966766357422 uV (normal site). Channel 6 Upper lip orbicularis – D – sEMG S – CVM 514151077270508 uV (paralisys side).
Fig. 2Segment labial before implant prothesis
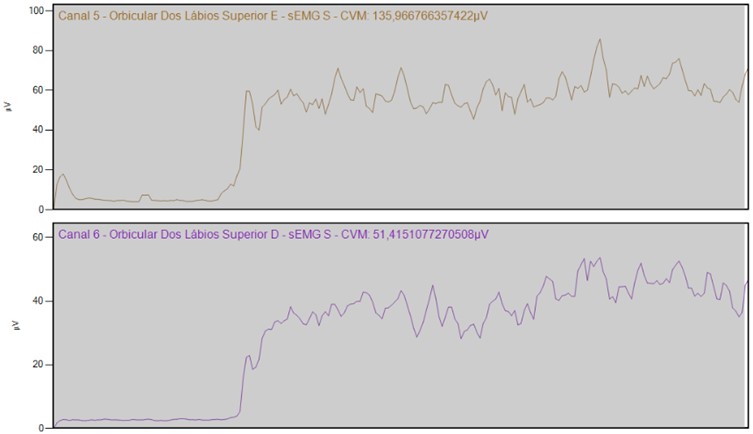
a)
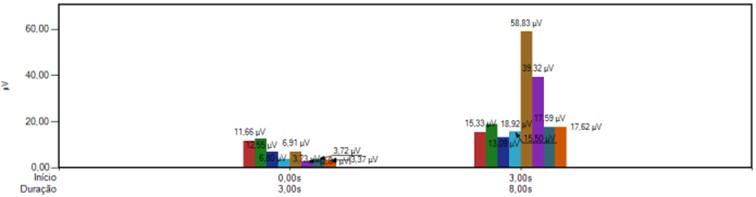
b) EMG average per contraction
Fig. 2 shows that The Electromyography re-evaluation of the Orbicular muscles of the Lips’ surface (bilateral) in maximum contraction, after the implant prosthesis. According to observation from the contralateral side, the normal would be IEMG of normality 0.79 to 1.28 [10]. Current IEMG: 0,66.
The value remains below normality, but closer to the normality value in relation to the initial assessment. After implant prosthesis this index rose to 0.66; even being below normality shows a IEMG closer to the normal range which starts at 0.79.
Fig. 3Extraoral photographs before and after the installation of implant prosthesis

a) The face in rest before implant prosthesis

b) The face in rest before implant prosthesis

c) The face in movement before the implant prothesis

d) The face in movement after the implant prothesis

e) Upper prosthesis

f) Lower prosthesis

g) Prothesis in occlusion
The paralyzed side (right side), through the dental contacts offered by the implant prothesis, during rest (Fig. 3), was able to offer more opposition to the force exerted by the healthy side. The contour of the lip and the groove naso labial became more harmonious, as well as the filter became less decentralized.
In Fig. 3, shows that during the movement the force exerted by the healthy side (left side) is still extremely powerful.
The clinical observations presented in this study were effectively proven by the photographs immediately after the installation of the implant protheses.
The eye contour of the paralyzed side (Right side) has become more natural.
The unilateral paralyzed face leads to a very accentuated asymmetry. The paralyzed and edentulous face aggravates even more because the paralyzed side does not offer opposition to healthy muscles, hindering speech and even more chewing and swallowing. Surface electromyography was used as a marker of the change in the performance of the facial muscles in the presence and absence of contact of the occlusal platform offered by the implant prothesis.
4. Conclusions
An effective dental contact, from the upper arch against the lower, during swallowing and chewing was important to avoid the excessive traction of the healthy side (left side) over the paralyzed side (right side).
What was found with the evaluation of surface electromyography, where it was noticed an increase in the IEMG index in the lip segment after the installation of the prosthesis.
The rehabilitation through prosthesis over implants was important in the harmonization of the paralyzed face, in the re-establishment of masticatory function and in the patient's quality of life.
References
-
J. W. House and D. E. Brackmann, “Facial nerve grading system,” Otolaryngology-Head and Neck Surgery, Vol. 93, No. 2, pp. 146–147, May 2016, https://doi.org/10.1177/019459988509300202
-
Thomas Von Arx, Marc J. Nakashima, and Scott Lozanoff, “The face – a musculoskeletal perspective. a literature review,” Swiss Dental Journal, Vol. 128, No. 9, pp. 678–688, Sep. 2018.
-
M. H. Hohman and T. A. Hadlock, “Etiologia, diagnóstico e tratamento da paralisia facial: 2.000 pacientes em um centro de nervo facial,” Laringoscópio, Vol. 124, No. 7, pp. 283–293, 2014.
-
R. F. Bentol, Doenças do Nervo Facial. São Paulo, 1998.
-
R. Queiroz, J. R. G. Testa, J. L. B. Santos, and F. J. M. M. Macedo, “O ajuste oclusal no tratamento da Paralisia Facial – Ensaio Clinico Randomizado Controlado,” Revista da APCD, Vol. 74, No. 2, pp. 145–154, 2020.
-
C. Werner, M. J. Sauders, E. Paunovich, and C.-K. Yeh, “Odontologia geriátrica,” Revista da Faculdade de Odontologia de Lins (Impresso), pp. 62–70, 1998.
-
M. J. Batista, H. P. Lawrence, and M. D. L. Rosário de Sousa, “Impact of tooth loss related to number and position on oral health quality of life among adults,” Health and Quality of Life Outcomes, Vol. 12, No. 1, pp. 1–10, Nov. 2014, https://doi.org/10.1186/s12955-014-0165-5
-
J. Finsterer, “Management of peripheral facial nerve palsy,” European Archives of Oto-Rhino-Laryngology, Vol. 265, No. 7, pp. 743–752, Mar. 2008, https://doi.org/10.1007/s00405-008-0646-4
-
M. Schimmel, T. Ono, O. L. T. Lam, and F. Müller, “Oro‐facial impairment in stroke patients,” Journal of Oral Rehabilitation, Vol. 44, No. 4, pp. 313–326, Mar. 2017, https://doi.org/10.1111/joor.12486
-
D. F. F. Bernardes, M. V. S. G. Gomez, and R. F. Bento, “Eletromiografia de superfície em pacientes portadores de paralisia facial periférica,” Revista CEFAC, Vol. 12, No. 1, pp. 91–96, Nov. 2009, https://doi.org/10.1590/s1516-18462009005000052
-
D. Bernardes, R. Bento, and M. Goffi Gomez, “The contribution of surface electromyographic assessment for defining the stage of peripheral facial paralysis: flaccid or sequelae stage,” International Archives of Otorhinolaryngology, Vol. 22, No. 4, pp. 348–357, Oct. 2017, https://doi.org/10.1055/s-0037-1607335
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Marcio Pelegrina – validation. Daniele Fontes – formal analysis. José Ricardo Gurgel Testa – supervision. Fabiana Augusto Novo Borghi – validation and visualization.
The authors declare that they have no conflict of interest.
Patient shown in the manuscript signed consent form allowing the use of the images.
